CT Simulation
Computer Tomography (CT) Scanning & Simulation allows the cancer specialists to design a treatment plan specifically for the patient based on the size, location, and shape of the tumor. The patient will have three-dimensional images (CT Scans) taken. These are used with the treatment planning software that helps determine how to best deliver the radiation beams while reducing damage to surrounding areas. In some cases, it may be necessary to mark the patient’s skin with a tiny marker so that the patient is perfectly realigned in the correct position for every session of radiation therapy. The need for a temporary or permanent marker will be discussed with the patient before the simulation.
Intensity-Modulated Radiation Therapy (IMRT)
Intensity-modulated radiation therapy (IMRT) is an advanced form of external radiation treatment that allows precise targeting of tumor cells. The CT simulator localization scan or other three-dimensional images provide the radiation oncologist with an understanding of the shape and location of the tumor. With 3D planning, the radiation oncologist specifies the dose from various beams and sums up those doses to calculate the dose to tumor and normal tissue (forward planning).
With IMRT, the radiation oncologist specifies the dose desired to give the tumor and the doses acceptable to the normal tissues (as low as possible). Then the computer system provides millions of alternative beam positions and the varying intensities of each beam, comparing one plan to the next until the best plan is identified. This is called inverse planning. Since each beam is broken up into many sub-beams of varying intensity the process is called intensity-modulated radiation.
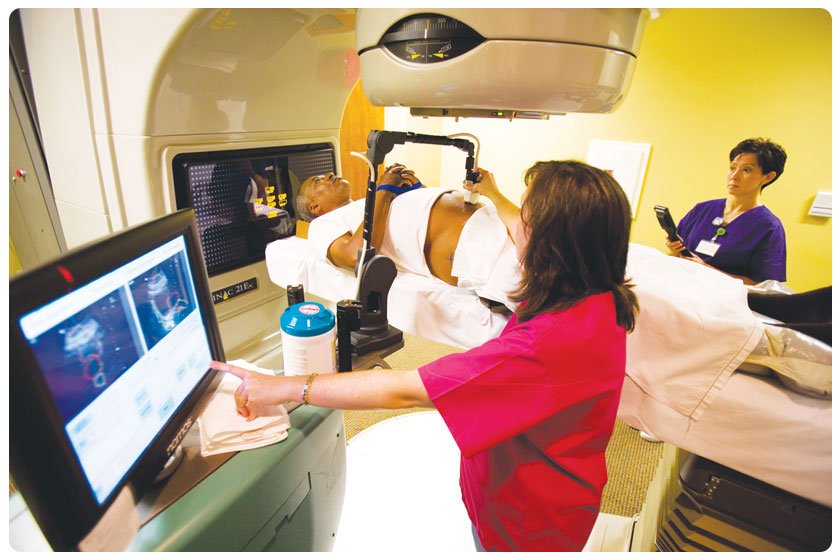
Image-Guided Radiation Therapy (IGRT)
Image-Guided Radiation Therapy (IGRT) combines three-dimensional images, such as CT scans, with the precise technology of either 3-D or intensity-modulated radiation therapy (IMRT) to pinpoint and treat cancerous tumors. The images allow the cancer specialists to precisely localize the tumor each time radiation therapy is administered. This improves both accuracy of delivery and safety by reducing radiation exposure to other areas of the body including nearby tissue and organs. IGRT is used to treat tumors in areas of the body that are prone to movement, such as the lungs, liver, and prostate gland, as well as tumors located close to critical organs and tissues.
Cone Beam CT
Cone Beam CT is typically used to map the tumor in the oral cavity, or to check for dental decay or periodontal disease that must be addressed before the start of radiation treatment. The machine produces a cone-shaped x-ray beam that is rotated around the head to produce three-dimensional images of the patient's teeth, bones, nerve pathways, and soft tissues. A cone beam CT is not the same as a conventional CT, but the images produced are very similar.
Barrigel
Barrigel® Hyaluronic Acid Rectal Spacer can help minimize prostate radiation side effects by temporarily positioning the rectum away from the prostate. When inserted, Barrigel creates space between the prostate and the rectum, moving the healthy organ out of radiation beam exposure. Because of its unique sculptable nature, Barrigel remains soft during insertion, allowing radiation oncologists to sculpt the spacer in place to create an optimal fit for your body. Barrigel is the only gel spacer than can be viewed clearly on ultrasound, the imaging machine used to guide your doctor’s placement during the procedure. This added visibility during insertion provides Dr. Agarwal and Dr. Shumway greater control and precision over the placement of the spacer.
SpaceOAR
While external radiation therapy is a proven prostate cancer treatment, it can also come with side effects— one of which is damage to the rectum. To reduce exposure of nearby organs to radiation, and to reduce the risk of side effects, our radiation oncologists may recommend the use of SpaceOAR® Hydrogel.
SpaceOAR® is a soft gel-like synthetic material that expands and creates space between the prostate and rectum. It is implanted prior to radiation treatment through a minimally invasive, outpatient procedure. The gel remains in place for about three months during radiation treatment and then liquefies, is absorbed, and cleared from the body through your urine.
Dr. Agarwal and Dr. Shumway specialize in SpaceOAR® placement and will be happy to answer any questions you may have regarding the procedure.
BioProtect
During radiation therapy, rectal toxicity can occur. To reduce the risk of damage to the rectal wall and other healthy tissue, our radiation oncologists may suggest using the BioProtect Balloon Spacer.
Ultrasound guides the insertion of a balloon in a minimally invasive procedure with local or general anesthesia. After inserting the balloon, it will be filled with saline and positioned to create a separation between the prostate and the rectum. This separation allows for safer and faster radiation therapy, while also improving your quality of life.
The BioProtect Balloon Implant maintains its shape and positioning throughout radiation treatment, and it naturally degrades over time. Additionally, it is visible under all imaging modalities, including CT, MRI, and ultrasound.
Stereotactic Body Radiotherapy (SBRT)
Stereotactic body radiotherapy (SBRT) is an advanced type of radiation therapy that delivers high doses of radiation using several beams of varying intensity aimed at a very targeted area of the body. Due to the high intensity of the radiation dose, only one to five treatments are given over a period of 1 to 5 days.
Stereotactic Radiosurgery (SRS)
Stereotactic radiosurgery (SRS) is an advanced type of radiation therapy that is a non-surgical procedure and requires no incision. SRS delivers precisely-targeted radiation at much higher doses than traditional radiation therapy, which can preserve surrounding healthy tissue. SRS is ideal for treating areas that cannot be treated with traditional surgical methods, such as inoperable brain tumors.
Low Dose Rate Brachytherapy
Low-dose rate (LDR) brachytherapy delivers radiation using a radioactive device or implant placed inside the body. The device delivers a low dose of radiation to a limited area over a period of 20 to 50 hours. It is one of the most focused, precise forms of radiation therapy and spares much of the surrounding tissue. LDR can be used to treat various cancer sites, such as prostate, uterus, or cervix.
Pluvicto®
Pluvicto, also known as lutetium Lu 177 vipivotide tetraxetan, is a recently approved treatment option for prostate cancer. This targeted radioligand therapy is specifically designed to treat prostate-specific membrane antigen-positive metastatic castration-resistant prostate cancer (PSMA-positive mCRPC), which is a type of advanced cancer. Pluvicto may also be used to treat cancer in the soft tissues and bones, as well as prostate cancers that are resistant to other anticancer treatments.